Nasal Spray VS Injectable Vaccines: The Differences you Need to Know
Dr. Melody Leung, Division of Life Science, tells us the differences between nasal spray and injectable vaccines.
By Dr. Melody Leung, Division of Life Science, HKUST
When we talk about vaccination, we often think of poking a metallic needle into our upper arm muscle, a method known commonly as intramuscular injection. Recently, we have also seen vaccines come in the form of a nasal spray, as the government last year allowed eligible residents to receive a free influenza vaccine by injection or via a nasal spray. Previously, we have discussed the three types of injectable vaccines available now to combat Covid-19 (The previous article: How much do you know about COVID-19 vaccines?). In the meantime, scientists are also developing one in the form of a nasal spray. So how does a nasal spray vaccine differ from others available via intramuscular injection?

Differences between a Nasal Spray Vaccine and Injectable Vaccine
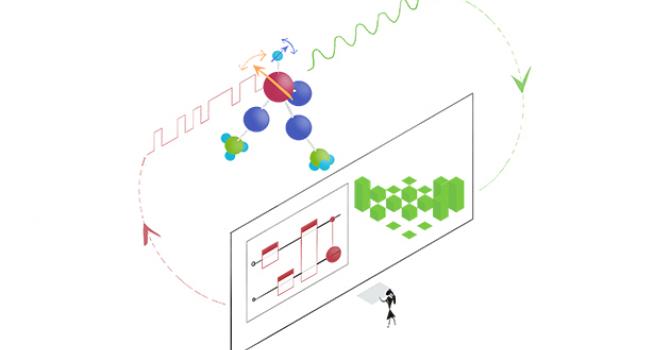
Nasal spray vaccines are created with live-attenuated viruses. With this method, the viruses are still alive and would reproduce inside our body, but as these viruses were prescreened and modified, they could no longer pose a threat to our health. When the vaccine is sprayed inside our nostrils, the live-attenuated viruses will go into our mucous membranes and start reproducing. Our body will falsely consider that the membranes are infected, and the mucosal-associated lymphoid tissues in our nostrils will trigger an immune response immediately to prevent our respiratory system from getting infected. When the immune cells “patrol” in our circulatory system, they will attack and neutralize the virus they come across. Given the above, a nasal spray vaccine gives a more comprehensive protection to the human body.
On the other hand, traditional injectable vaccines are created with inactivated viruses. As these viruses are already dead, they have lost the ability to reproduce in our body, which would then make them harder to be detected by our body’s immune system. To enhance and stimulate an immune response, an immunological adjuvant is often added into the vaccines, but generally speaking, the response is still weak and may require an individual to receive multiple injections in order to obtain sufficient immunity. As these inactivated vaccines, or any other newer types, are injected directly into our muscles, they will not be able to generate an immune response from the lymphoid tissues in our nostrils, and as a result, they will not provide protection to our respiratory system. If our body is infected via our nose, we can then only wait until the immune cells in our circulatory system to discover and destroy the viruses in their usual “patrol” routine.

Developments of Covid-19 Nasal Spray Vaccine
Currently, scientists from around the world are conducting research on a Covid-19 nasal spray vaccine, such as researchers from the University of Hong Kong and the Lancaster University in the United Kingdom. As Covid-19 is a highly contagious novel virus that has infected millions of people, the development of vaccines is essentially a race against time. With limited time available, many teams have chosen to forego the process of prescreening and modifying, which would make the Covid-19 virus presented in their vaccines to become live-attenuated. Instead, the new Covid-19 nasal spray vaccine will use other live-attenuated viruses as a carrier, infused with gene coding for the spike protein of the Covid-19 virus. When sprayed into our nostrils, the infected mucosal-associated lymphoid tissues will create the corresponding spike proteins based on the genotypes of the Covid-19 virus, and our body will create a memory of these proteins and subsequently, generate an immune response. The current Covid-19 nasal spray vaccine developed by the University of Hong Kong uses genetically modified and live-attenuated influenza virus as a carrier, which would give recipients double protection against both influenza and Covid-19. The Lancaster University version of the vaccine uses live-attenuated Newcastle Disease Virus as a carrier.
Can vaccines deal with virus variants?
When viruses enter our body, our immune system issues an immune response and produce immunoglobulin (Ig), more commonly known as antibodies, to attack the intruders. There are multiple types of Ig, such as IgG, which is often produced in our circulatory system; and then there is IgA, which is created in the immune system in our nose. Interestingly, IgA has proven to be effective against multiple strains of virus, which means that even if the infecting COVID-19 virus presents a different version of spike protein, IgA can still respond and prevent this virus from entering our mucous membranes and lower respiratory system, which could lower our chance of getting infected. In comparison, IgG would only respond to a prescribed type of virus and its characteristics found in a vaccine. If a virus variant surfaces with different characteristics, then the particular IgG vaccine may lose its effectiveness against it.
Storing the Vaccines
As live-attenuated vaccines rely on the virus to reproduce inside a human body and subsequently generating an immune response, they must be kept and stored in a temperature range between 2-8 °C. If not handled properly (e.g. keeping the storage temperature too low, repetitive defrosting and freezing, or exposing the vaccine for a long period of time before use at over 25 °C), the reproduction ability of these live-attenuated viruses would lower substantially rendering the vaccines useless.